Unpacking the Link Between PCOS & Insulin Resistance
You may have heard the term ‘insulin resistance’ used in conjunction with Polycystic Ovary (Ovarian) Syndrome (PCOS), but what actually is it and how is it relevant to PCOS? How can I find out if I am insulin resistant? In today’s blog, we unpack the link between PCOS & insulin resistance.
First, lets take a minute to revise a little bit about PCOS and insulin resistance.
What is PCOS?
Polycystic Ovary (Ovarian) Syndrome (PCOS) is a complex hormonal condition which impacts between 8-13% , with some studies showing up to 20%, of women. Based on the Monash International PCOS Guidelines (1,) PCOS is diagnosed using the Rotterdam criteria. You need to meet at least 2 out of 3 of the following:
· Absent or anovulatory periods (may be >40 days or more frequent)
· Clinical and/or biochemical signs of high androgens such as acne, hirsutism and/or hair loss.
· Polycystic ovaries on ultrasound (1.)
The cause of PCOS is unknown, however, appears to be driven by the imbalance of hormones, including an excessive production of androgen hormones (such as testosterone) and resistance to the hormone insulin (2.) This imbalance can drive symptoms, including irregular periods, weight gain, hair loss, acne and unwanted hair growth (2.)
So, what actually is insulin resistance?
What is insulin resistance?
You may have heard of insulin before. You may associate it with the fact that some people with diabetes need to take it to survive… But what does it actually do in the body?
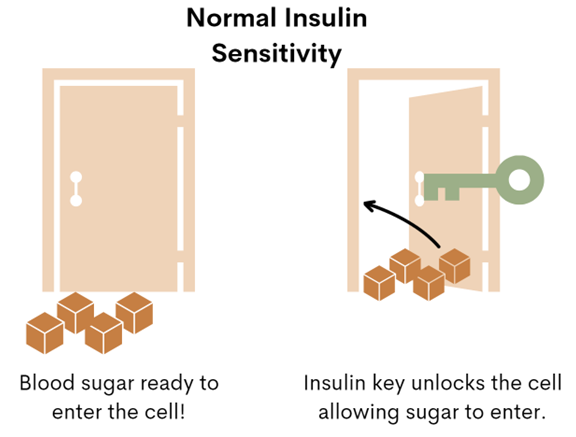
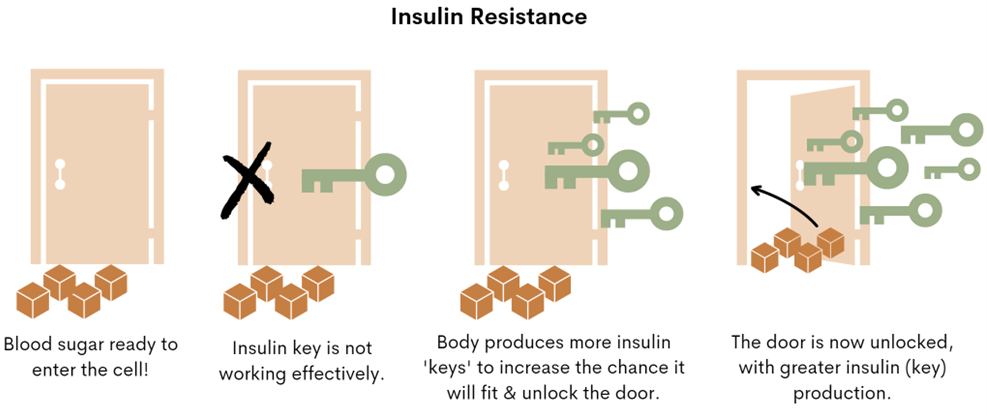
Insulin is the key responsible for ‘unlocking’ the door to our body’s cells, allowing sugar (glucose) to move from the blood, into the cell. When you are resistant to insulin, this means your body’s cells do not respond as effectively to the insulin ‘key.’ So, what does the body do? The body produces more of it, hoping that one of the insulin keys will fit and unlock the door to allow the sugar (glucose) to move from the blood, into your cells where it can be used for energy. See diagram 1 for more!
Diagram 1 – Normal Insulin Sensitivity
Diagram 2 – Insulin Resistance
So, how does insulin resistance relate to PCOS?
Insulin resistance frequently occurs in those with PCOS. Insulin resistance can drive symptoms such as:
Carb cravings
Weight gain (particularly around the middle)
Skin tags
Dark skin patches, known as acanthosis nigricans
Irregular cycles.
Research has shown that between 75-95% of women with PCOS have insulin resistance, irrespective of body size (3.)
High insulin and insulin resistance can also contribute to high androgen levels and high androgen levels can worsen insulin resistance, contributing to symptoms such as acne, irregular cycles and hirsutism (unwanted hair growth.)
This is why one of the backbone of PCOS management is addressing underlying insulin resistance.
So, now we know insulin resistance is important to consider, how can we find out if we are insulin resistant?
How can I find out if I am insulin resistant?
If you have PCOS, I recommend working with a doctor and dietitian to help you identify if you are insulin resistant. Some of the following tests may be ordered to identify if you have insulin resistance:
Fasting Insulin: this measures how much insulin is circulating in the blood after a period of fasting. If high, this may indicate insulin resistance.
Fasting Glucose: this measures how much glucose is circulating in the blood after a period of fasting. If high, this may indicate insulin resistance.
HbA1c: this measures your average blood sugar level over 3 months.
HOMA-IR: this is calculated using your fasting insulin & fasting glucose results. Your doctor and/or dietitian can assist you in working this out.
Based on your results, your doctor may also recommend an Oral Glucose Tolerance Test (OGTT) if necessary.
Some additional tests which may be relevant includes a blood lipid panel which assesses your ‘bad’ cholesterol (LDL-C), ‘good’ cholesterol (HDL-C) and triglycerides. High LDL-C, high triglycerides and/or low HDL-C may also be an indicator of insulin resistance, in conjunction with some of the above tests (4.)
I found out I am insulin resistant, what now?
If you have found out you are insulin resistant, do not worry – with the right support and changes, you can improve your insulin sensitivity, reduce your risk of developing type 2 diabetes and ultimately better manage your PCOS symptoms. So, what are some simple strategies you can start with?
Modify the types of carbohydrates you are eating: swap processed / refined carbohydrates for whole grain low GI carbohydrates, such as swapping white bread for a whole grain bread e.g. Bakers Delight Prebiotic Cape Seed Bread or a Burgen bread, like their Whole Grain & Quinoa Bread.
Start your day with a high fibre, high protein breakfast: Aim for at least 25g protein at breakfast paired with fibre and a healthy fat to stabilise your blood glucose (sugar) levels across the day.
Go for a 10-15 minute walk after each meal: this has been shown to improve blood glucose control and insulin sensitivity (5.)
Include resistance activity: on 3-4 days per week: such as weightlifting.
Pair carbohydrates with a source of protein and healthy fats: such as having whole grain toast with avocado and eggs.
Modify carbohydrate portions: a dietitian can help you modify your carbohydrate portions and distribution across the day to support optimal blood glucose (sugar) control and insulin sensitivity.
Consider nutritional supplements*: work with a qualified dietitian to determine if supplementation is required, such as the use of Inositol (40:1 ratio of Myo & d-chiro inositol)
See a dietitian: Navigating insulin resistance is complex and tailored advice and support can make it MUCH easier to manage. Book a free discovery call today to learn how Lettuce Talk Nutrition can support you or apply to our 16 Week PCOS Nutrition Coaching Program or Insulin Resistance coaching program.
The advice provided in this article is in a general nature only. For personalised advice, please apply to our 16 Week PCOS Nutrition Coaching Program or book a discovery call to learn about our 1:1 consultations.
Note on supplements: please work with a qualified dietitian when starting nutritional supplements. The type, dosage and requirements in relation to supplements vary between individuals. Supplementation may be contraindicated and side effects may occur if supplementing without the support of a professional. Always notify your doctor when commencing new nutritional supplements.
References
1. Witchel SF, Oberfield SE, Peña AS. Polycystic Ovary Syndrome: Pathophysiology, Presentation, and Treatment With Emphasis on Adolescent Girls. J Endocr Soc. 2019 Jun 14;3(8):1545-1573. doi: 10.1210/js.2019-00078. PMID: 31384717; PMCID: PMC6676075.
2. International evidence-based guideline for the assessment and management of polycystic ovary syndrome 2018: https://www.monash.edu/__data/assets/pdf_file/0004/1412644/PCOS_Evidence-Based-Guidelines_20181009.pdf
3. Stepto NK, Cassar S, Joham AE, Hutchison SK, Harrison CL, Goldstein RF, Teede HJ. Women with polycystic ovary syndrome have intrinsic insulin resistance on euglycaemic-hyperinsulaemic clamp. Hum Reprod. 2013 Mar;28(3):777-84. doi: 10.1093/humrep/des463. Epub 2013 Jan 12. PMID: 23315061.
5. Loretta DiPietro, Andrei Gribok, Michelle S. Stevens, Larry F. Hamm, William Rumpler; Three 15-min Bouts of Moderate Postmeal Walking Significantly Improves 24-h Glycemic Control in Older People at Risk for Impaired Glucose Tolerance. Diabetes Care 1 October 2013; 36 (10): 3262–3268. https://doi.org/10.2337/dc13-0084